Indexed In
- Open J Gate
- Genamics JournalSeek
- ResearchBible
- Electronic Journals Library
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- Virtual Library of Biology (vifabio)
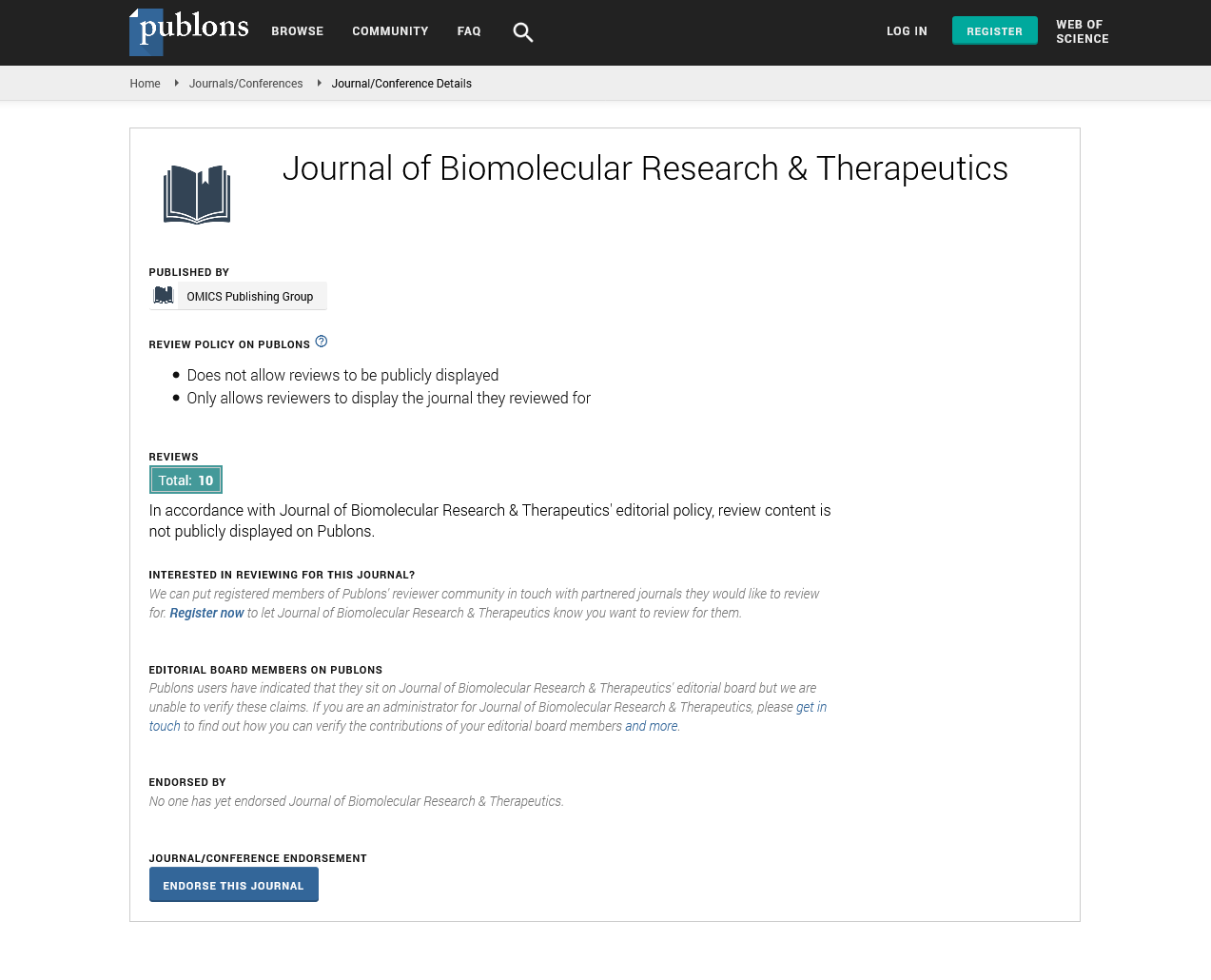
- Publons
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Requirement of optimized Time dependent Drug delivery system for management of gastric acid Diseases
P. D. Juyal
Gastroesophageal reflux disease (GERD), also known as acid reflux, is a long-term condition in which stomach contents rise up into the esophagus, resulting in either symptoms or complications.[5][6] Symptoms include the taste of acid in the back of the mouth, heartburn, bad breath, chest pain, regurgitation, breathing problems, and wearing away of the teeth. Complications include esophagitis, esophageal stricture, and Barrett's esophagus.
Risk factors include obesity, pregnancy, smoking, hiatal hernia, and taking certain medicines. Medications involved may include antihistamines, calcium channel blockers, antidepressants and sleeping pills. Acid reflux is due to poor closure of the lower esophageal sphincter, which is at the junction between the stomach and the esophagus. Diagnosis among those who do not improve with simpler measures may involve gastroscopy, upper GI series, esophageal pH monitoring, or esophageal manometry.
Treatment options include lifestyle changes; medications; and sometimes surgery for those who do not improve with the first two measures. Lifestyle changes include not lying down for three hours after eating, raising the head of the bed, losing weight, avoiding foods which result in symptoms, and stopping smoking.[5] Medications include antacids, H2 receptor blockers, proton pump inhibitors, and prokinetics.
In the Western world, between 10 and 20% of the population is affected by GERD. Occasional gastroesophageal reflux without troublesome symptoms or complications is even more common. The classic symptoms of GERD were first described in 1925, when Friedenwald and Feldman commented on heartburn and its possible relationship to a hiatal hernia. In 1934 gastroenterologist Asher Winkelstein described reflux and attributed the symptoms to stomach acid.
In recent years, many attempts have been made to enhance the drug bioavailability and therapeutic effectiveness of oral dosage forms. In this context, various gastroretentive drug delivery systems (GRDDS) have been used to improve the therapeutic efficacy of drugs that have a narrow absorption window, are unstable at alkaline pH, are soluble in acidic conditions, and are active locally in the stomach. In this review, we discuss the physiological state of the stomach and various factors that affect GRDDS. Recently applied gastrointestinal technologies such as expandable, superporous hydrogel; bio/mucoadhesive, magnetic, ion-exchange resin; and low- and high-density-systems have also been examined along with their merits and demerits. The significance of in vitro and in vivo evaluation parameters of various GRDDS is summarized along with their applications. Moreover, future perspectives on this technology are discussed to minimize the gastric emptying rate in both the fasted and fed states. Overall, this review may inform and guide formulation scientists in designing the GRDDS. The main mechanism of acid suppression by using PPI is they block the gastric H,K-ATPase, inhibiting gastric acid secretion and it produces enables healing of peptic ulcers, gastro esophageal reflux disease (GERD) Barrett’s Esophagus.
But it was reported that 24 hrs. Acid secretory studies suggest that maintaining the gastric acid ph. above 3 or 4 for 18 hrs. helps to 100 % duodenal ulcer healing in 4 week treatment and 100 % gastric ulcer in 8 weeks and for erosive esophagitis 20- 22hrs per day maintain the ph. above 4.[2]
PPI cannot inhibit all proton pumps through oral route of administration because PPI has low half-life (about 90 Min). In 24 hours again 20 % new PPI get synthesized. And mainly these newly PPI synthesized at the night time as compared to day time. So the bedtime administration of proton pump will not inhibit proton pump through nocturnal acid breakthrough. Because drug disappear after sometime. Increasing the dose of drug it does not produce any effect but split dose repeatedly produces effect.[1] So to administered dose of PPI twice a day is more effective as compared to the single large dose for maintain the ph. above 4.[2]
The main problem of PPI administration is to educate the people for administration of PPI to produce more effect; also compliance of patience towards the PPI is more important if for more effect dose split in twice a day patient compliance get hampered. And a chance of dose missing is more.
During night time if patient administered dose then it get disappear after some time and the 20% new synthesized proton pump release the gastric acid because they are not inhibited by PPI due to short half-life of the drug. To inhibit this newly synthesized proton pump next dose of drug is required but at night time it’s not shows patient compliance. So if the newly synthesized drug produces the acid then may the chances of gastric refluxes and disturbance of sleep at early morning.
So to overcome above problem, develop suitable drug delivery system which can deliver the required amount of drug after single dose administration is very important. This can inhibit the PPI, which are previously activated and also inhibit the PPI which get synthesized during night time.
Missed dose of PPI may again increase the Ph. above 4. But this system release drug after period of time and maintain the pH of esophagus below 3 or 4. This helps to cure the duodenal ulcer, erosive esophagitis.
So the design and optimization of such dosage forms which reduce the complications of dose administration, maintain esophagus ph. above 4, reduce the dose administration frequency, and inhibit the PP which get synthesized at night time. This will definitely help to treatment of gastric acid Diseases and improve the patient compliance.
Published Date: 2020-12-25; Received Date: 2020-12-20