Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
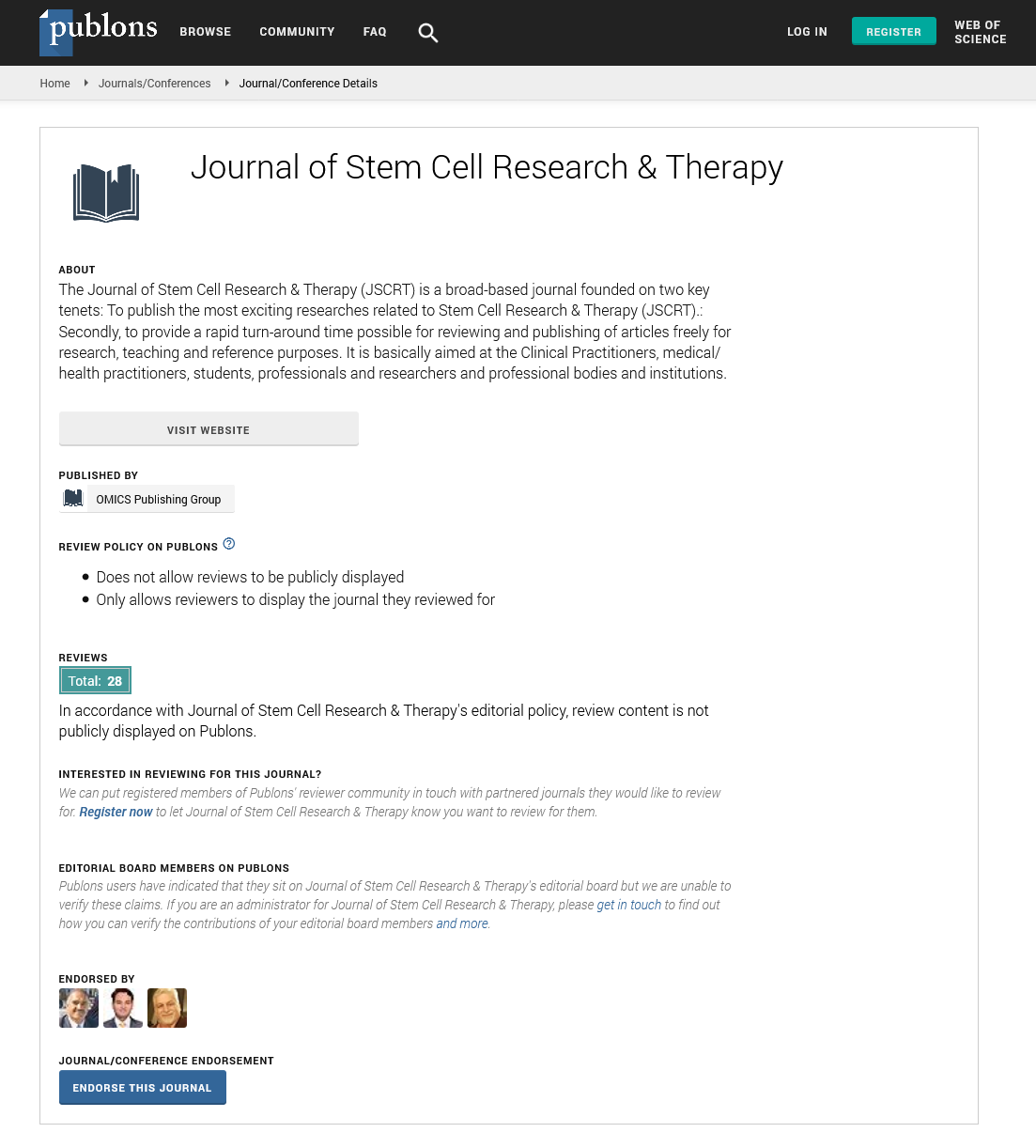
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Modalities to Improve Cord Blood Engraftment
Meral Beksac and Pinar Yurdakul
Umblical cord blood (UCB) is one of the major sources of Hematopoietic Stem Cell Transplantation (HSCT) with increasing use in clinical practice. UCB can be a life saver for patients who do not have a matched unrelated adult donor or for patients who are in need of an urgent transplantation. Various factors make UCB a significant source of Hematopoietic Stem Cells (HSCs), including ease of procurement and lack of donor attrition, with the ability to process and long term storage of donor cells. Importantly, UCB donations can be used right away without the need for a “perfect” HLA match, thereby increasing donor access to HSCT, particularly for minority and mixed ethnicity patients, for whom a suitably matched related or unrelated donor may be difficult to locate. The major limitation of UCB is the quantity of cells to be infused. Although high proliferative potential allows one log less use of HSCs (HSC<105/kg) compared to bone marrow (BM) or peripheral blood mononuclear cells (PBSC), even this amount cannot be reached in the majority of patients under donor search. When total nucleated cell (TNC) and CD34+ cell doses in UCB grafts are analyzed, a high correlation is observed with the rate of neutrophil and platelet engraftment, the incidence of graft failure and early transplant-related complications. It has been shown that UCB grafts with more than 3/6 HLA mismatches and with cell doses under the defined minimum threshold lead to higher transplantation related mortality (TRM). Especially when adult cord blood transplantation (UCBT) is the subject, providing units with enough cells remains the major drawback. Despite certain efforts, there is still an unmet need for increasing HSC cell dose and/or stimulating engraftment without loss of their long term repopulating (LTR) potential and reducing graft versus host disease (GVHD). Intrinsic and extrinsic cellular factors have been proven to act roles in HSC expansion thus justifying their role in in vitro and ex vivo culture conditions. Attempts to regulate these factors through ex vivo expansion methods aim to overcome insufficient cell numbers while methods promoting HSC homing is in favor of the latter. Combination of both appear to work synergistically. Induction or adoptive transfer of UCB derived immune cells particularly Natural Killer (NK) cells and regulatory T cells (T reg) with or without cytokines are also effective approaches for gaining better engraftment levels after UCBT. All of these approaches have been denoted as “successful” in pre-clinical in vitro and animal studies. Many of them have also been tested in early/later phase clinical trials resulting in encouraging results. We aim to review the current knowledge on UCB expansion and engraftment enhancer methods, a very rapidly improving field particularly in the last decade.