Indexed In
- Open J Gate
- Genamics JournalSeek
- Academic Keys
- JournalTOCs
- China National Knowledge Infrastructure (CNKI)
- Ulrich's Periodicals Directory
- RefSeek
- Hamdard University
- EBSCO A-Z
- Directory of Abstract Indexing for Journals
- OCLC- WorldCat
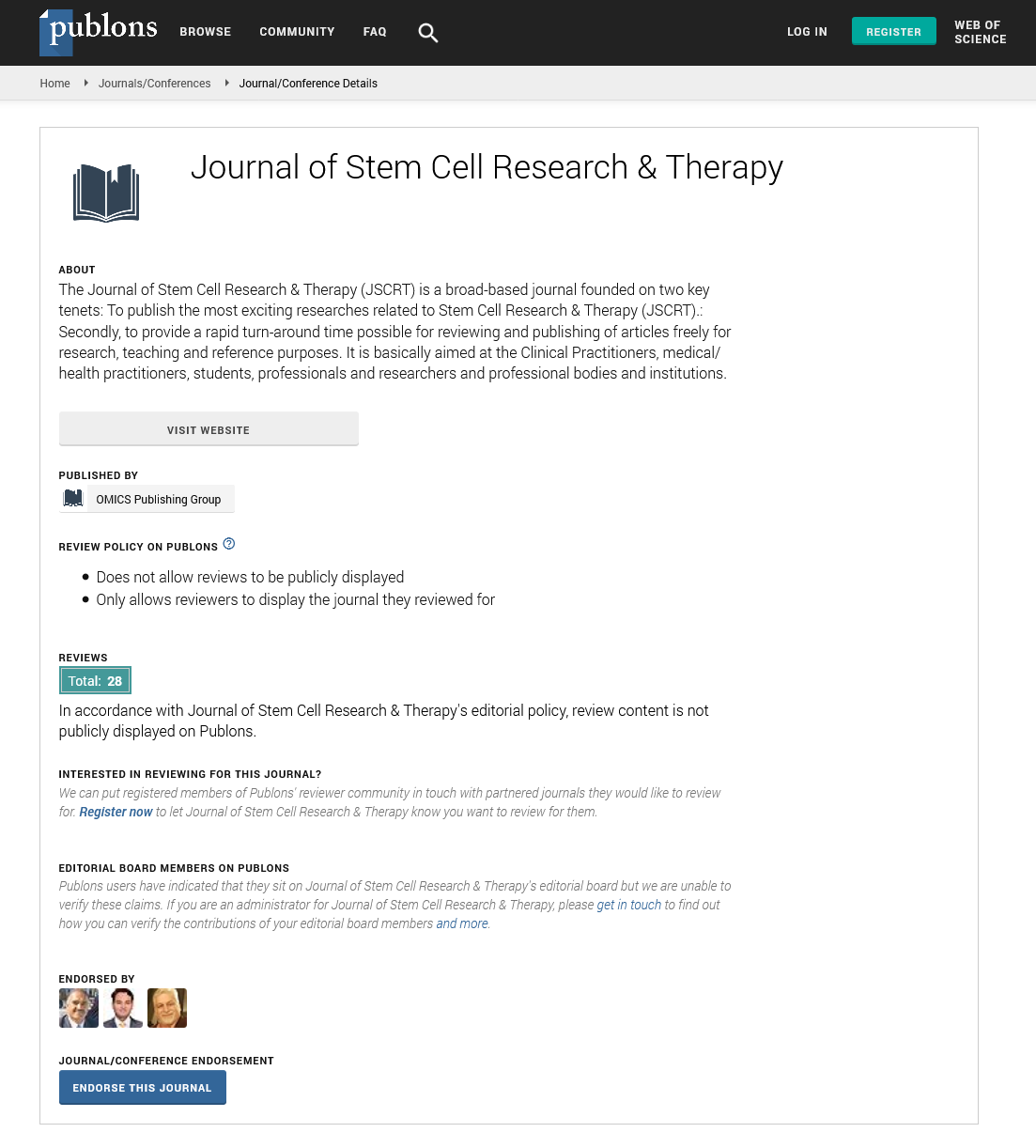
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Cell-Based Therapies for Peripheral Arterial Disease
Yasuyuki Fujita and Atsuhiko Kawamoto
Chronic critical limb ischemia (CLI) is defined as the end-stage of lower limb ischemia due to atherosclerotic peripheral arterial disease (PAD) or vasculitis including thromboangitis obliterance (Buerger’s disease). CLI patients are at very high risk of amputation and experience poor physical function, leading to severe morbidity and mortality despite the development of surgical bypass technique or endovascular approach. Therefore, exploring novel strategies for blood flow recovery of ischemic limbs is urgently needed for patients with CLI. Although researchers initially focused on gene therapy using proangiogenic growth factors, recent discovery of somatic stem/progenitor cells including bone marrow (BM)-derived endothelial progenitor cells (EPCs) and mesenchymal stem cells (MSCs) has drastically developed the field of therapeutic angiogenesis for CLI. In 2002, the first clinical trial of intramuscular injection of BM-derived mononuclear cells (BM-MNCs) demonstrated safety, feasibility and efficacy for CLI patients. Since then, at least 50 clinical trials of BM- and peripheral blood (PB)-derived MNC therapy, 4 trials of CD34+ cell (an EPC-enriched fraction) therapy and 8 trials of MSC therapy have been performed for CLI. Overall, the results of these early phase clinical trials regarding stem/progenitor cell therapies may be safe, feasible and effective. However, only few late-phase clinical trials have been conducted. Currently, at least 3 phase III trials including 2 trials using BMMNCs and 1 trial using granulocyte-colony stimulating factor (G-CSF)-mobilized PB-MNCs are ongoing. This review provides an overview of the preclinical and clinical reports to demonstrate the usefulness and the current limitations of the cell-based therapies.