Indexed In
- Open J Gate
- Cosmos IF
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
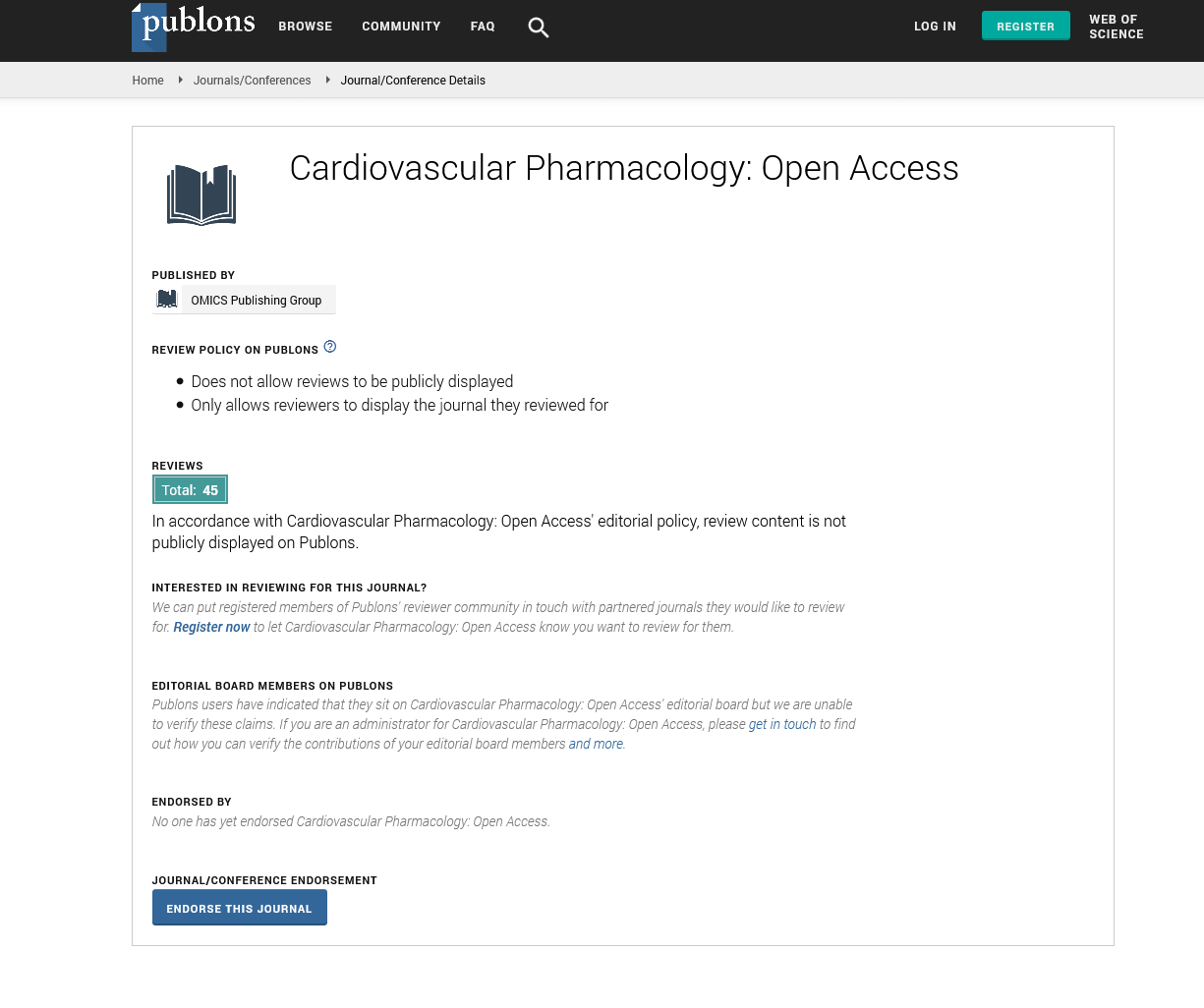
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
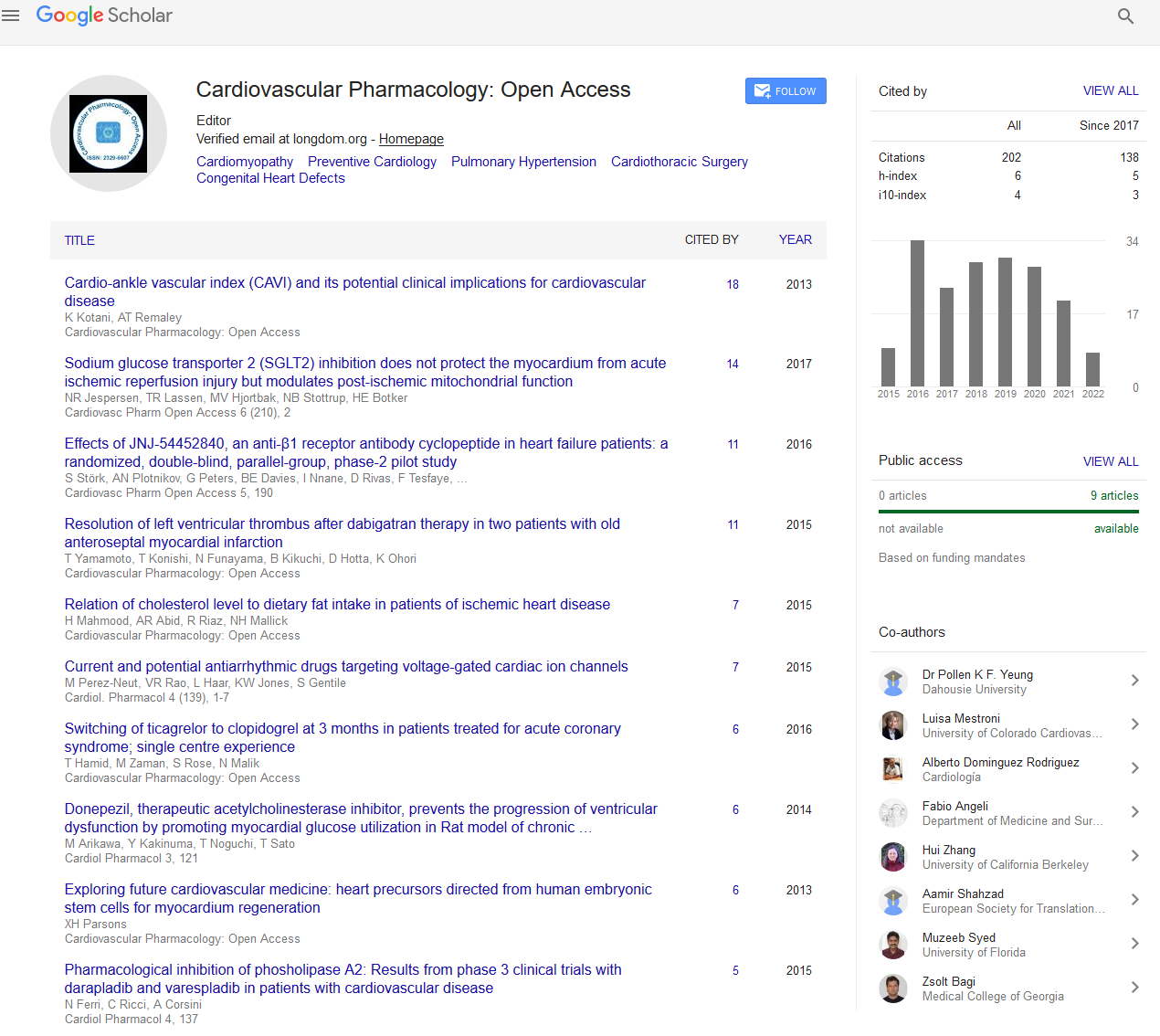
- Google Scholar
Useful Links
Share This Page
Journal Flyer

Open Access Journals
- Agri and Aquaculture
- Biochemistry
- Bioinformatics & Systems Biology
- Business & Management
- Chemistry
- Clinical Sciences
- Engineering
- Food & Nutrition
- General Science
- Genetics & Molecular Biology
- Immunology & Microbiology
- Medical Sciences
- Neuroscience & Psychology
- Nursing & Health Care
- Pharmaceutical Sciences
Abstract
Acquired ventricular septal rupture with surgical minimally invasive occlusion
Ventricular septal defect (VSD) is the most common congenital heart disease[1]. Acquired VSD is very rarely, ventricular septal rupture (VSR) is a rare complication of blunt chest trauma (BCT) in children [2-4].
An 1-year, 9-month-old male child presented with a 5-hour history of blunt chest trauma. The infant underwent emergency bedside echocardiography, the results were as follows: muscular ventricular septal defect with funnel-shaped, and the left and right ventricular shunt orifice diameter were 1.0 cm and 0.5 cm respectively, color doppler flow imaging showed a bidirectional shunt between the left and right ventricles (figure1) , severe tricuspid regurgitation, mild pulmonary hypertension, a small amount of pericardial effusion, the thickness of the myocardium was uneven and in wedge-shaped, which was opposite to the muscular ventricular defect. the width of the widest part was about 1.1 cm, the narrowest part was about 0.57 cm, the thickness of the thinnest part was 0.3 cm, and the left ventricular wall was slightly dilated on repeat echocardiogram. The electrocardiogram showed pathological Q wave, ST segment elevation. Chest computed tomography showed double lung contusion.
Muscular portions of ventricular septal defect was occluded by transesophageal echocardiogram guided, left ventricular posterior wall aneurysm was repaired, mitral valvuloplasty and foramen ovale suture closure were performed under cardiopulmonary bypass. During the operation, it was found that the ventricular septal defect was about 1.0 cm from the apex, right ventricular shunt was 0.6cm, and two openings were adjacent to left ventricular surface, 0.6 cm above and 0.3 cm below. The opposite left ventricular posterior wall of the ventricular septal defect was slightly bugling outward, it felt apparently uneven in thickness with a sense of cleavage and the length was about 1.5 cm. On the left ventricular view, the anterior papillary muscle showed partial chordae tendinosa ruptured, anterior mitral valve prolapsed, and the edge was floating. Both immediate transesophageal and transthoracic echocardiogram showed no residual shunt after operation. At half-month of follow-up, the case remained symptom free. On the 16th day after operation, blood oxygen saturation decreased, the lowest was 27%, he was in critical condition, and tracheal intubation was performed, the laboratory showed severe anemia. His patients decided to give up treatment.
Published Date: 2021-05-21;